63 years old known case of polycythemia on treatment. Recently developed secondary myelofibrosis.
63 years old known case of polycythemia on treatment. Recently developed secondary myelofibrosis. Now patient presented with cognitive decline and speech difficulty with paresthesia of right hand.
On examination:
- No motor or sensory deficits
- No ataxia
- Difficulty in articulating and expressing
Patient was advised to undergo MRI brain with IV contrast and cervical spine screening.
Protocol: Multiplanar multisequence imaging of the brain was performed with IV contrast.
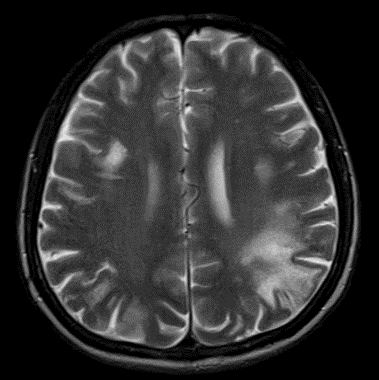
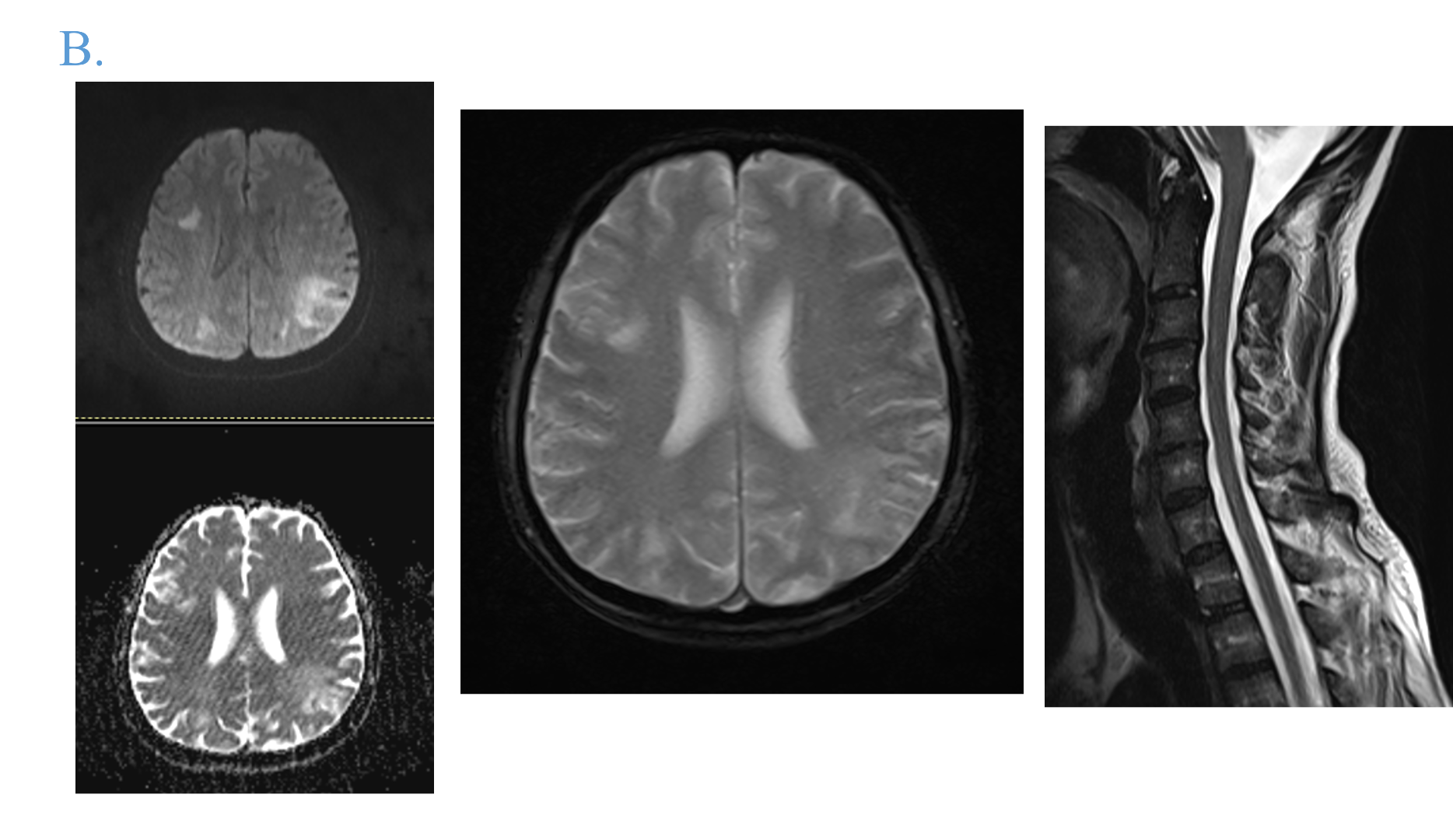
A.
- Multiple bilateral white matter T2 hyperintensities involving centrum semiovale and corona radiata. These appear asymmetric with involvement of the subcortical U fibres (yellow arrows). No mass effect noted.
- Involvement of the splenium of corpus callosum seen (blue arrow).
- No significant enhancement in post contrast T1 sequence. No other enhancing lesions or abnormal meningeal enhancement noted as well.
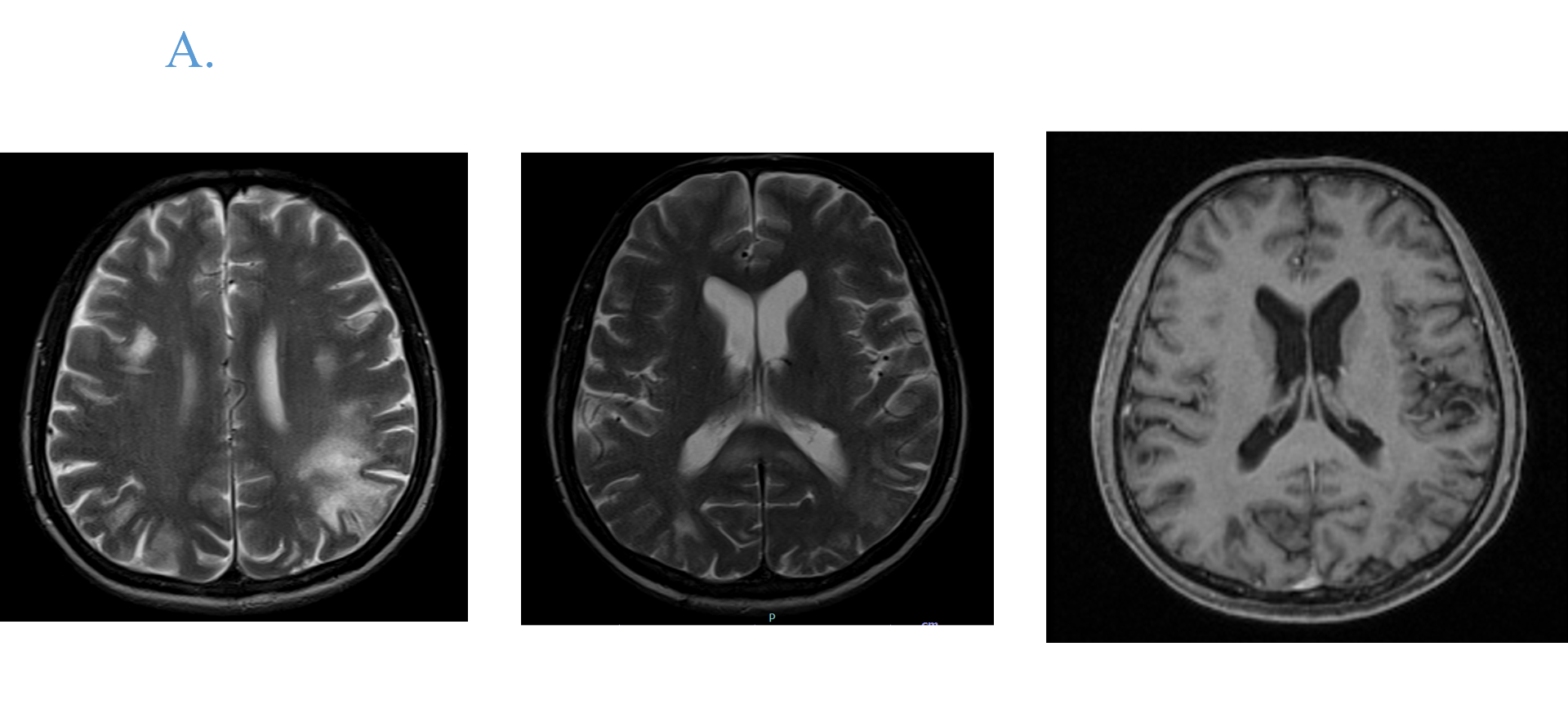
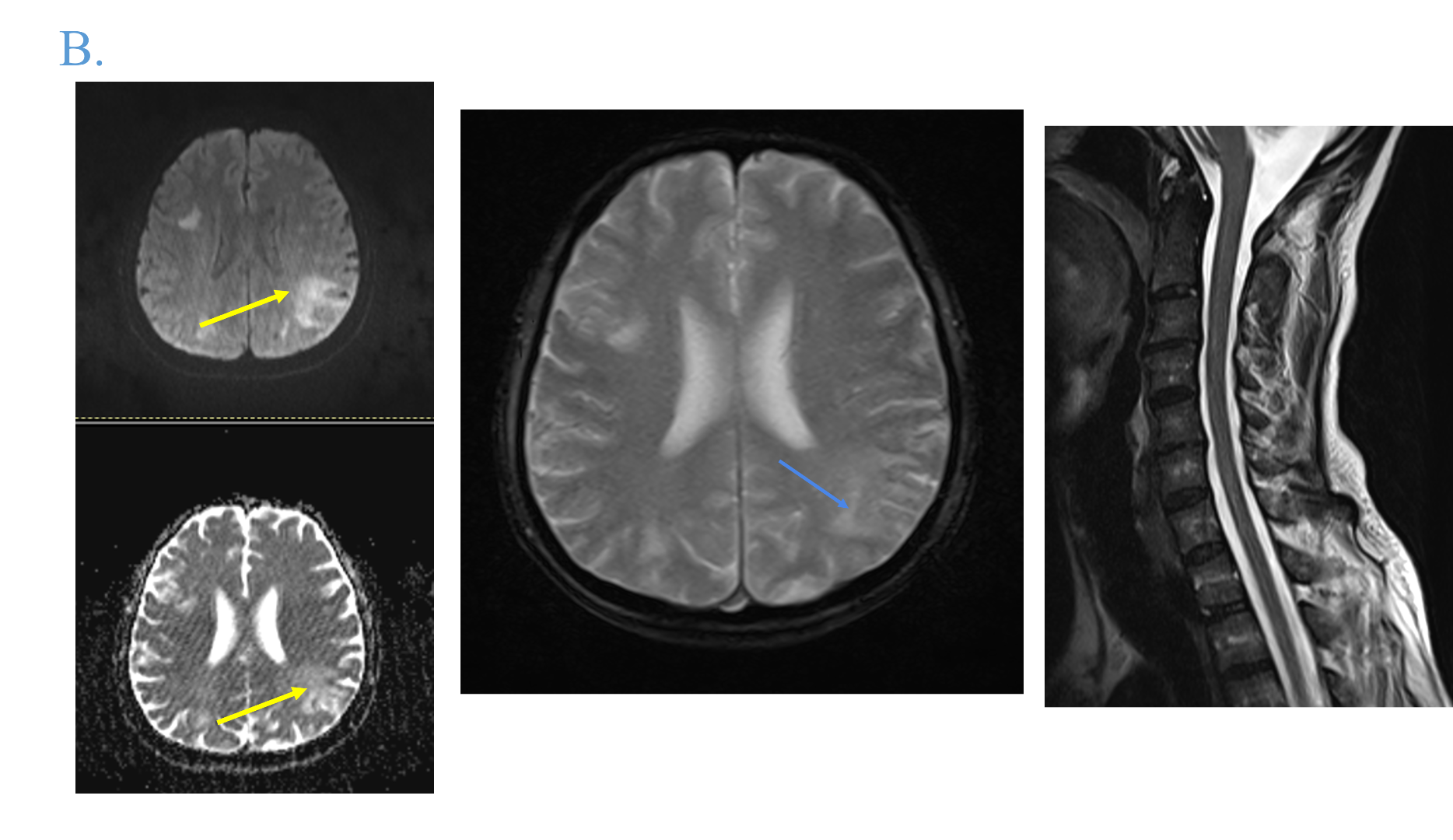
B.
- These lesions show facilitated diffusion, appearing hyperintense on DWI and ADC images (blue arrows).
- No blooming on SWI to suggest blood products or calcifications.
- Cervical spine screening is unremarkable.
Progressive multifocal leukoencephalopathy considering the immune compromised status
CSF study revealed JC virus DNA; thus, confirming the radiological diagnosis.
DISCUSSION:
Progressive multifocal leukoencephalopathy (PML) is an opportunistic infection of the CNS caused by the JC virus, which infects white and grey matter cells and leads to irreversible demyelination and neuroaxonal damage (1).
JCV, a member of the Polyomaviridae family, was first isolated from the brain of a patient with Hodgkin disease in 1971 (2). Inhalation and ingestion of contaminated water have been suggested as major modes of transmission of the virus (3). Suppression of cellular immunity, secondary to HIV infection, is the major cause of the JCV reactivation and constitutes approximately 80% of patients with PML. Other less common immunodeficiency settings for PML are hematologic malignancies (13%), organ transplant recipients (5%), and autoimmune diseases treated with immunomodulators (3%) (4).
PML is the most common manifestation of JCV infection.
JC virus associated pathologies
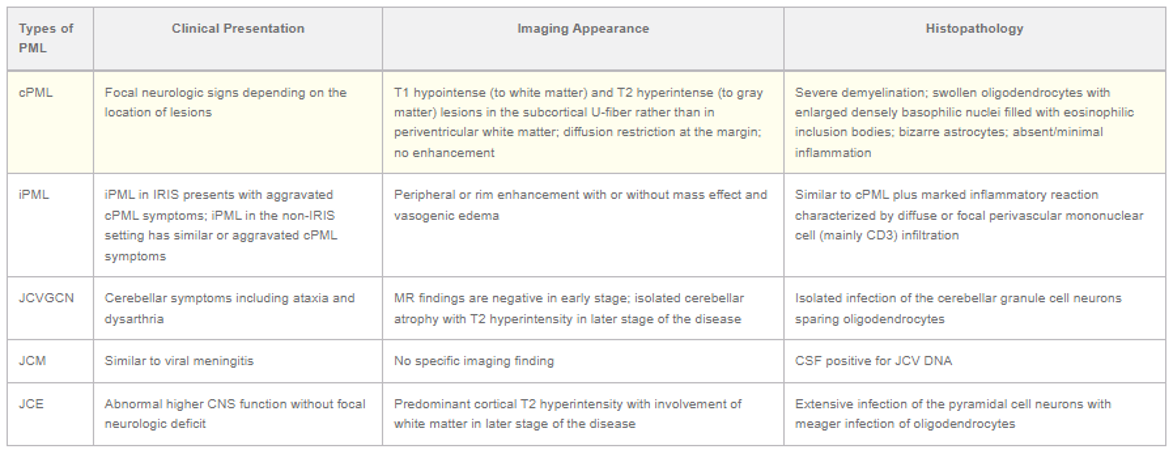
Courtesy – A.K Bag et al
IMAGING OF PML
- Confluent, bilateral asymmetrical T2/FLAIR hyperintense and T1 hypointense white matter. Basal ganglia, corpus callosum, brainstem and cerebellum also can be involved (5). No mass effect. Mild diffusion restriction and patchy enhancement may be present at the periphery, but predominantly non restricting and non enhancing.
- MRS may show reduced NAA with elevated choline, lipid and lactate. Leading edge can show increased perfusion.
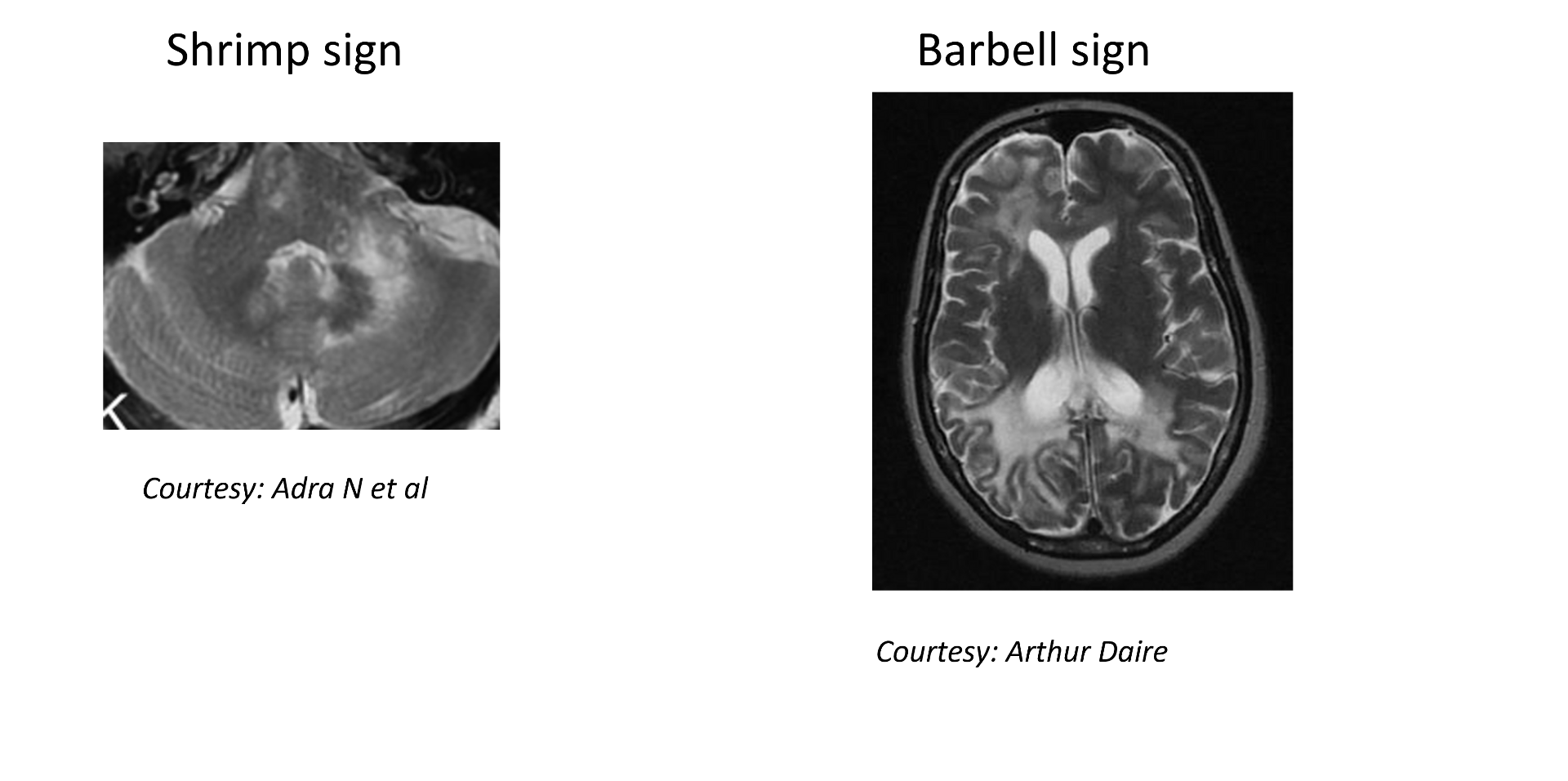
Named signs on T2
- Barbell sign – bilateral parieto-occipital lesions crossing midline with involvement of splenium of corpus callosum (6)
- Shrimp sign – cerebellar involvement with dentate nucleus sparing (7)
Subcortical U fibre and corpus callosum involvement are important diagnostic clues.
Differentials
- HIV Encephalopathy – usually symmetric with atrophy ( PML is asymmetric)
- PRES – parieto-occipital with different clinical course, may involve grey matter
- MS, ADEM – open ring enhancement diffusion restriction, spinal cord involvement
REFERENCES
- Baldassari LE, Wattjes MP, Cortese ICM, Gass A, Metz I, Yousry T, Reich DS, Richert N. The neuroradiology of progressive multifocal leukoencephalopathy: a clinical trial perspective. Brain. 2022 Apr 18;145(2):426-440. doi: 10.1093/brain/awab419. PMID: 34791056; PMCID: PMC9630710.
- Padgett BL, Walker DL, ZuRhein GM, Eckroade RJ, Dessel BH. Cultivation of papova-like virus from human brain with progressive multifocal leucoencephalopathy. Lancet i: 1257–1260.
- Bofill-Mas S, Formiga-Cruz M, Clemente-Casares P, Calafell F, Girones R. Potential transmission of human polyomaviruses through the gastrointestinal tract after exposure to virions or viral DNA. Journal of virology. 2001 Nov 1;75(21):10290-9.
- Gheuens S, Pierone G, Peeters P, Koralnik IJ. Progressive multifocal leukoencephalopathy in individuals with minimal or occult immunosuppression. Journal of Neurology, Neurosurgery & Psychiatry. 2010 Mar 1;81(3):247-54.
- Bag AK, Curé JK, Chapman PR, Roberson GH, Shah R. JC virus infection of the brain. American Journal of Neuroradiology. 2010 Oct 1;31(9):1564-76.
- Bezuidenhout A, Andronikou S, Ackermann C, Du Plessis A, Basson D, Bhadelia R. "Barbell Sign": A Diagnostic Imaging Finding in Progressive Multifocal Leukoencephalopathy. J Comput Assist Tomogr. 2018;42(4):527-30.
- Adra N, Goodheart AE, Rapalino O, Caruso P, Mukerji SS, González RG, Venna N, Schmahmann JD. MRI shrimp sign in cerebellar progressive multifocal leukoencephalopathy: description and validation of a novel observation. American Journal of Neuroradiology. 2021 Jun 1;42(6):1073-9.
Dr RAHUL KARTHIK L
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr ANAGH VISHNU NARAYANAN
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.