A 45 years, old female patient presented with complaints of insomnia, impaired memory, behavior changes, confusion, progressive psychosis and urinary incontinence.
A 45 years, old female patient presented with complaints of insomnia, impaired memory, behavior changes, confusion, progressive psychosis and urinary incontinence. Patient experienced myoclonus of both hands and eyelids.
Non contrast MRI OF THE BRAIN
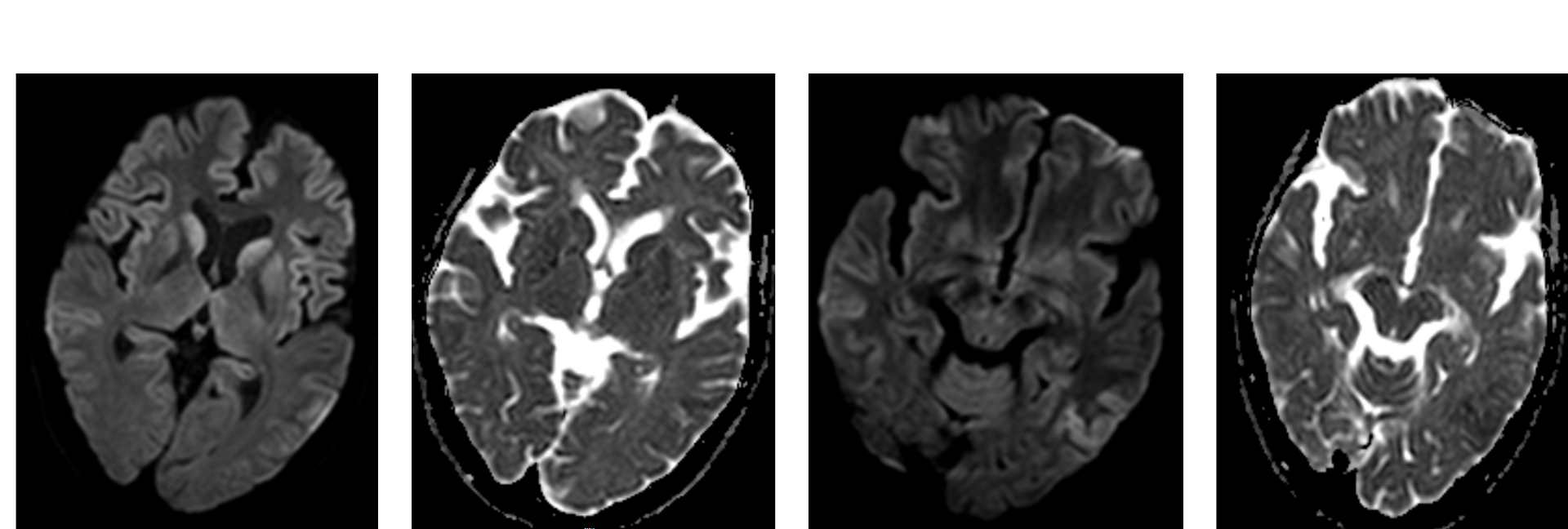
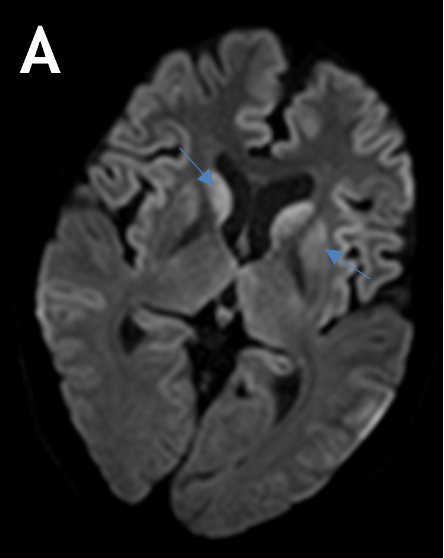
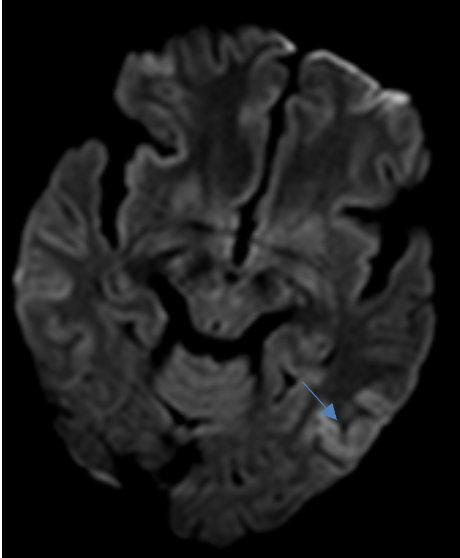
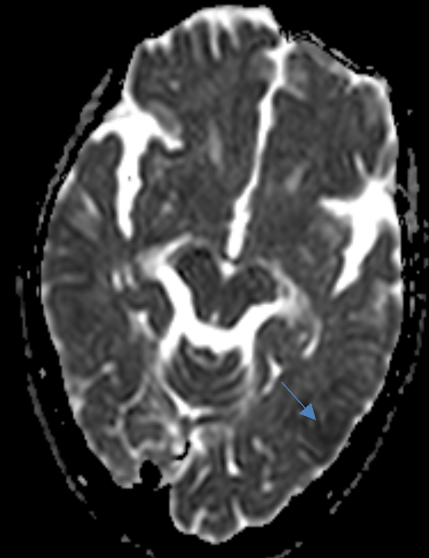
- A. Axial diffusion weighted and corresponding ADC images at the level of basal ganglia and at the level of mid brain.
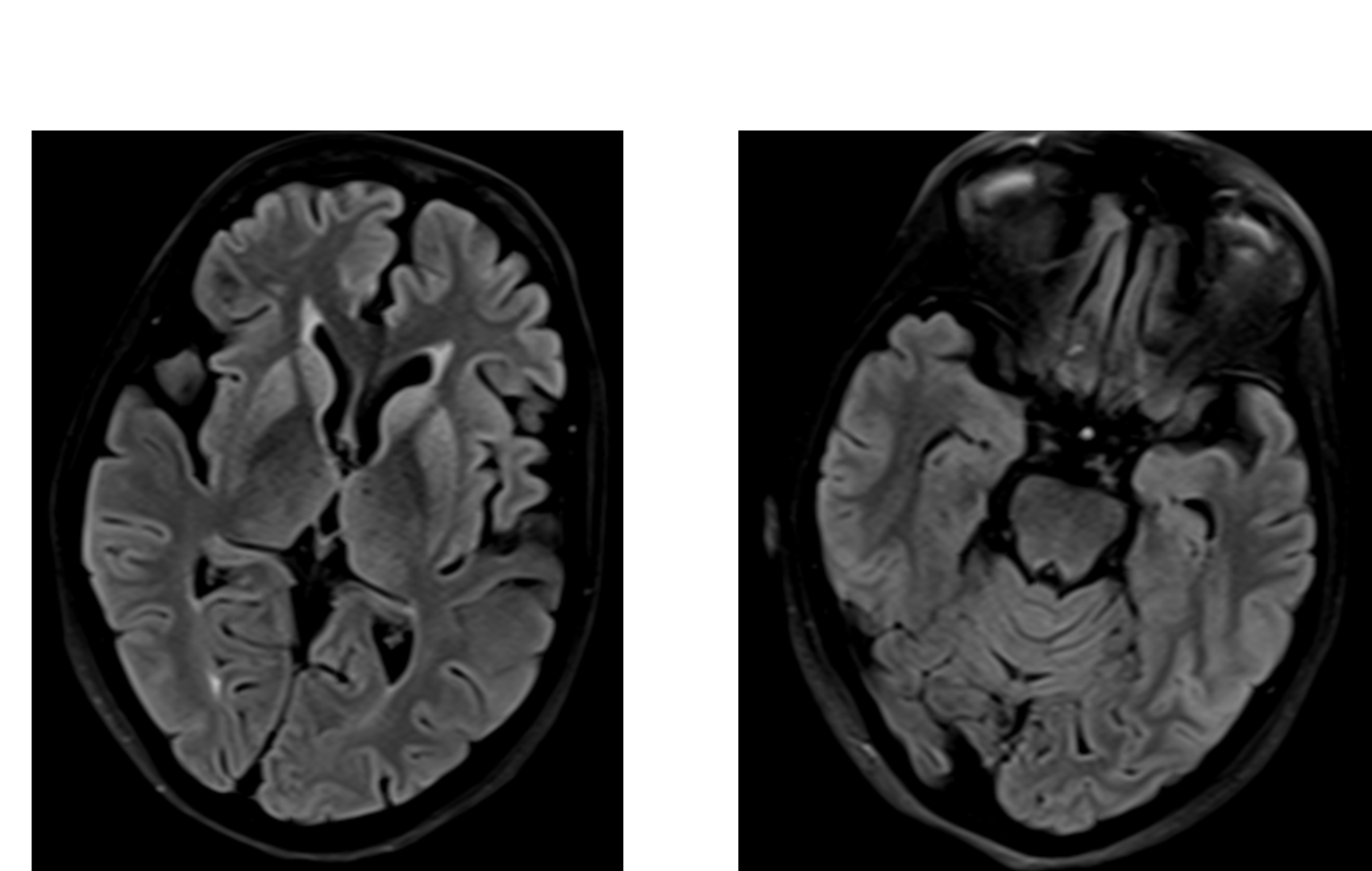
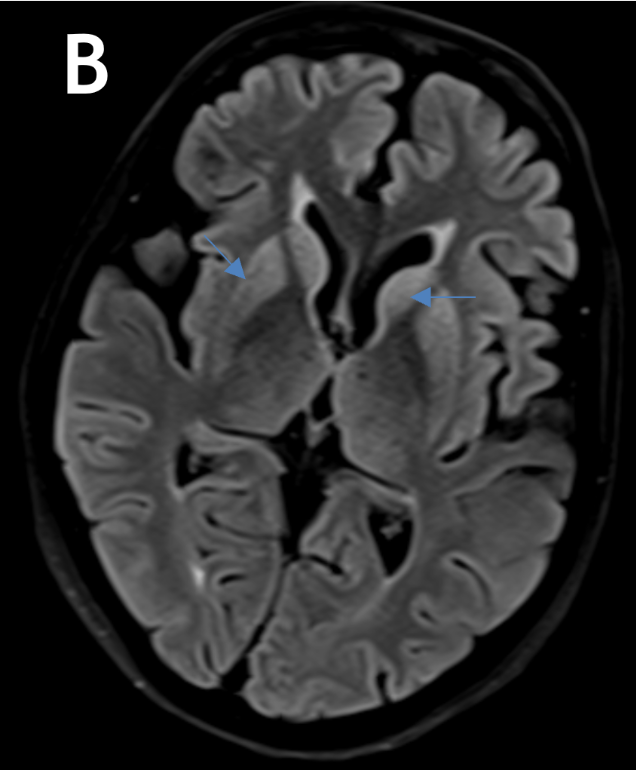
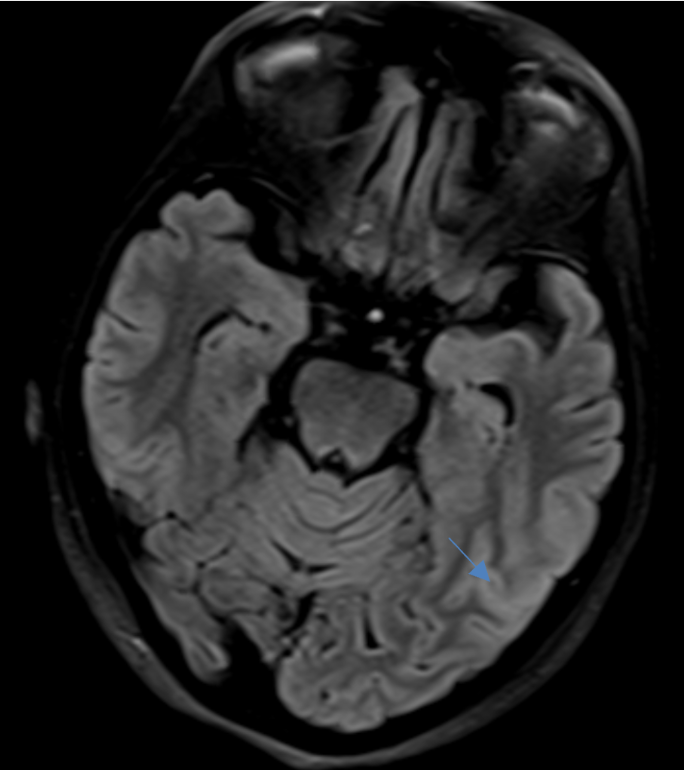
- B. Axial FLAIR images at the level of basal ganglia and at the level of mid brain.
- A. Axial diffusion weighted and corresponding ADC images at the level of basal ganglia and mid brain show, Restricted diffusion in bilateral caudate, putamen and in bilateral parietal and temporal cortex. Subtle diffusion restriction also noted in bilateral medial thalami.
- B. Axial FLAIR images at the level of basal ganglia and mid brain show, Hyperintensities in bilateral caudate, putamen, medial thalami and in bilateral parietal and temporal cortex.
Creutzfeldt-Jakob disease
DISCUSSION
- Creutzfeldt-Jakob disease (sCJD) is a very rare transmissible spongiform encephalopathy causing rapidly progressive dementia and death within 1 year of symptom onset.
- CJD is caused by a type of abnormal protein known as a prion or scrapie PrP.
- Types of Creutzfeldt-Jakob disease:
- Sporadic (sCJD)
- Variant (vCJD)
- Familial (fCJD)
- Iatrogenic (iCJD)
- The trio of laboratory tests commonly used in diagnosis are electroencephalography (EEG), cerebrospinal fluid (CSF), and brain magnetic resonance imaging (MRI).
CLINICAL SYMPTOMS
- of this disease are nonspecific and most commonly include rapidly progressive dementia, myoclonus, visual hallucinations, cerebellar dysfunction (such as ataxia and nystagmus), pyramidal or extrapyramidal signs (such as spasticity, rigidity, dystonia, or bradykinesia), and eventually akinetic mutism.
PATHOLOGY
- Creutzfeldt-Jakob disease is mediated via prions, a type of protein, which manifests in sheep as the disease scrapie, and in cows as bovine spongiform encephalopathy.
- Prion diseases are a heterogeneous assortment of neurodegenerative diseases characterized by alteration of a naturally existing prion protein (PrPc ) to an abnormal folded protein termed scrapie prion protein
- Prions are considered infectious in the sense that they can alter the structure of neighbouring proteins.
- Creutzfeldt-Jakob disease leads to spongiform degeneration of the brain, which is thought to be caused by the conversion of normal prion protein to proteinaceous infectious particles that accumulate in and around neurones and lead to cell death.
Diagnostic Markers
- CSF 14-3-3 protein: positive result in a patient suspected clinically of having sporadic Creutzfeldt-Jakob disease
- CSF and/or olfactory mucosa real-time quaking-induced conversion (RT-QuIC) seeding assays:
- Detects minute amounts of the disease-specific pathologic prion protein
- Found to be more sensitive than CSF 14-3-3 protein titres
- A definitive diagnosis requires a brain biopsy
IMAGING
- MRI is the modality of choice to assessing patients with suspected CJD.
- The most sensitive sequence to identify characteristic changes is diffusion-weighted imaging.
- sCJD patients can precede the onset of clinical manifestations, even in unsuspected cases with unremarkable/atypical results at EEG and CSF examination, making this technique(DWI) the cornerstone to support early diagnosis.
- Signal abnormalities may be subtle initially but become more pronounced as the disease progresses.
- Pattern of involvement:
- Cerebral cortex: Focal or diffuse, symmetric or asymmetric involvement Perirolandic area usually spared
- Basal ganglia: Symmetric or asymmetric involvement, particularly of caudate and putamen (anterior-posterior gradient)
- Cerebellum: Atropy
- DWI: hyperintensity including cortical ribboning, the hockey stick sign, and the pulvinar sign.
- ADC: variable, depends on timing
- early: low values - these may be seen prior to marked changes on DWI or visible FLAIR changes
- late: pseudonormalised or facilitated and associated with atrophy.
- T2/FLAIR: hyperintensity is more subtle than DWI changes and may be absent early in the course of the disease
- T1: may show high signal in globus pallidus (uncommon)
- T1 C+ (Gd): no abnormal enhancement
Dr. Sriram Patwari
Senior Consultant
Department of Radiology
Manipal hospital, Yeshwanthpur, Bengaluru.
Dr. Ram Sanjith V
Cross Section Fellow
Manipal hospital, Bengaluru.